 |
|
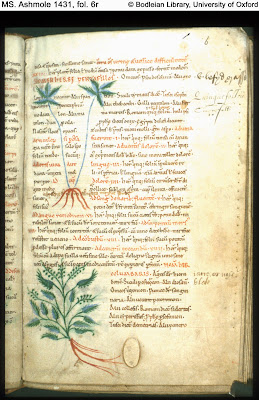
Pentafillos (Cinquefoil) and Columbaris (Vervain)
Bodleian MS Ashmole 1431, fol. 6r. The Old English
Herbarium credits Pentafillos,
or ‘fifleafe’ in Old English,
as a curative for anything from joint ache to stomachaches
and headaches to even ulcers. To the author’s knowledge,
however, the efficacy of fifleafe
in these recipes has not
been tested recently. |
Bald’s Leechbook is thought to be one of the earliest English medical texts, offering advice on diagnosis and treatment and a collection of recipes for herbal, animal, and mineral-based medications. This leechbook, along with the Old English Herbal (Herbarium) and Medicina de quadrupedibus, and the Lacnunga (a collection of recipes from a variety of sources), function as scholarly repositories and practical manuals for tenth and eleventh-century England. Moreover, the information in the leechbooks tends to follow a specific pattern: they begin with a table of contents and are structured from a “head-to-toe” manner for physical illnesses, before moving on to remedies for internal ailments. In his seminal book, Anglo-Saxon Medicine, M.L. Cameron states that these medical texts show that they “could take from the Greeks and Romans some of the best they had to offer and integrate that borrowing into an English tradition.”[3]
Based on Cameron’s analysis, the medical techniques of this period may have been more effective than had been previously recognized. The most significant of these, Cameron argued, was the remedy for a stye found in Bald’s Leechbook, which was just retested by microbiologist, Freya Harrison, and her team Steve Diggle, Alan Roberts, and Anglo-Saxonist Christina Lee, from the University of Nottingham, and Kendra Rumbaugh, from Texas Tech University:
Wyrc eagsealfe wiþ wænne: genim cropleac 7 garleac begea emfela, gecnuwa wel tosomne, genim win 7 fearres geallan begean emfela, gemeng wiþ þy leaces, do þonne on arfæt, læt standan nigon niht on þæm arfæt, awring þurh claþ 7 hlyttre wel, do on horn 7 ymb niht do mid feþere on eage; se betsta læcedom.[4]
Make an eye salve for a stye: take cropleac ‘onion’ and garlic equal amounts of both, pound well together, take wine and bull’s gall equal amounts of both, mix with the ‘leeks’, then put in a brass vessel, let stand for nine nights in the brass vessel, strain through a cloth and clear well, put in a horn and about night time put on the eye with a feather; the best remedy.[5]Cameron hypothesizes that the ingredients in the eye-salve prescription were likely to be helpful in combating and inhibiting the growth of bacteria, like staphylococcus.[6] However, replicating cures from Anglo-Saxon and medieval medicine can be problematic, especially when one term can be used to refer to multiple types of herbs, as Stephen Pollington notes.[7] Also, it is difficult to link Old English plant names to modern species, as climate and environmental factors have changed since the tenth century, altering current types of vegetation.[8] What’s more is that often the Anglo-Saxon prescriptions are vague in the quantities of each ingredient, and therefore these recipes have often been discounted or overlooked by modern researchers and scientists. When Barbara Brennessel, Michael Drout, and Robyn Gravel tested the eye-salve recipe in vitro against common disease-causing bacteria in 2005, they found these issues to be challenging in recreating an effective medication.[9] Their historic-pharmacological approach involved interpreting the Anglo-Saxon recipe, determining the specific ingredients and their quantities, and then testing the compounds on different bacteria strains in petri dishes, using the Kirby-Bauer method. While their version of the compound eye-salve recipe did not prove to be effective in their experiments, they did find that individual ingredients, such as oxgall, did inhibit growth of some types of bacteria.[10] Nonetheless, the approach by Nottingham researchers appears to be similar to the tests done by Brennessel, Drout, and Gravel, but the results of their interpretation of the Old English prescription produced more positive outcomes this time around.
One issue involving the study of Anglo-Saxon medical treatises is that the transcriptions and translations that are readily available are mostly from the mid-nineteenth century, like the one above by Oswald Cockayne. Cockayne was the first person to edit, transcribe, translate, and publish the Anglo-Saxon leechbooks in three volumes for the Rolls Series between 1864 and 1866. Several misconceptions of Anglo-Saxon medicine and culture were perpetrated while Cockayne’s edition remained the most accessible version, according to contemporary critics, such as Linda Voigts and Anne Van Arsdall.[11] Victorian audiences at the time of Cockayne were wary of medical recipes involving prayers, charms, and supernatural explanations. All of these are included in the leechbooks and are also present to a certain degree in many medieval and Renaissance medical treatises. Since this period, this early critical wariness has been frequently used as an excuse to write off earlier forms of scientific knowledge. Furthermore, it can be easy to see how aspects of anatomical descriptions and herbal prescriptions may seem foreign to modern physicians and scientists, as they are often rooted in humoral theory. Today doctors no longer ascribe to the notion of the four humors, and this is another reason medieval medical cures tend to be overlooked until they are translated into our modern notions of “scientific” practices. Though the recent experiments with the eye-salve cure have reached a wider audience in the news, this is not the first time that contemporary physicians, researchers, and Medievalists have turned to Anglo-Saxon medicine in hopes of re-discovering possible remedies for illnesses.
 |
|
Lupinum (lupine), depicted on left page, top right-hand side
Bodleian MS Ashmole 1431, fols 27v-28r. |
by modern standards, manganese (if at all effective) would represent a clumsy and potentially dangerous anticonvulsive. It is hard to imagine that lupines could serve as a remedy for acute, isolated seizures: while studies clearly point to systemic manganese concentration as a factor in seizure susceptibility, there is no evidence that direct manganese administration would immediately relieve a seizing patient. The Anglo-Saxon remedies call for lupines to be ingested, in any event, and manganese absorption in the small intestine would not begin for a number of hours. Supplementing the patient’s diet with manganese, however, might serve to raise the general seizure threshold, and thus reduce the frequency and intensity of future attacks.[14]
.jpg) |
|
Betonice (betony),
from 11th-century Old English
Herbarium in London,
BL Cotton Vitellius C. iii,
fol. 20r (facs). Held at Newberry Library, Chicago.
Photo credit: Sarah Gillette, 2015.
|
Likewise, Marijane Osborn assesses recipes associated with pregnancy and childbirth in Leechbook III and attempts to determine the degree to which the pharmacology of the flowering herbs that appear there might achieve the actual effects being sought by those women.[18] For example, if a woman has difficulty expelling the placenta after giving birth, one recipe from this leechbook recommends a hot drink made from boiled brooklime (Veronica beccabunga) in ale. Osborn states that brooklime can function as an emmenagogue, or a plant that promotes menstrual flow, and that the chemicals in this caudle would help expel a blocked placenta.[19] However, as researchers found with the eye-salve recipe, the exact herbal quantities and dosages of each treatment were probably transmitted orally from doctor to apprentice-in-training, instead of being included in written form. For this reason, herbs like brooklime, or pennyroyal, which is in a recipe that aids in expelling a dead fetus, can become extremely dangerous to women if misused. They, like the some of the other herbs mentioned above, are pharmakons and can either heal or poison the patient.
So how do we advance medicine, when faced with material that may provide answers but can be difficult to interpret, or may be missing crucial information due to a variety of reasons? In an interview, Christina Lee made some important points about interdisciplinarity and research: “modern research into disease can benefit from past responses and knowledge, which is largely contained in non-scientific writings. But the potential of these texts to contribute to addressing the challenges cannot be understood without the combined expertise of both the arts and science.”[20] Perhaps a new way of thinking is needed in order to understand and to relate earlier medical writings to our modern-day lives. It is true that Anglo-Saxon scholars have attempted to overcome earlier translations and criticism that sought to separate and emphasize the “rational” (“scientific” and “practical”) medicine from those elements which were judged to be “non-rational” (e.g., “supernatural” or “magical” or “literary”). However this mindset needs to encompass more than just an “either-or” methodology and taxonomy. Kelly L. Bezio and Ashley Reed note that “even the multi-disciplinary subfields […] tend toward the dyadic thinking of secularization: literature and medicine, medicine and religion, religion and literature. But these academic pair bonds rarely tell the whole story about an event or idea.”[21] Thus, we need to move beyond our entrenched modes of inquiry and seek a more global and interdisciplinary approach, all the while respecting the knowledge and culture of our ancestors.
Sarah Gillette
Ph.D. Candidate
English Department, Western Michigan University
Note: The first two images are from http://www.bodley.ox.ac.uk/dept/scwmss/wmss/medieval/mss/ashmole/1431.htm. The third image is from a facsimile of Cotton Vitellius C.iii owned by the Newberry Library and photographed by Sarah Gillette.
Manuscripts mentioned in this post:
- London, BL Royal 12, D xvii: Bald's Leechbook (Old English medical compendium). 10th-11th century. View at http://www.bl.uk/onlinegallery/onlineex/illmanus/harlmanucoll/m/011hrl000000055u00001000.html.
- London, BL Cotton Vitellius C.iii: Old English Herbarium and Medicina de quadripedibus. Early 11th century, Old English.
- London, BL Harley 585: Lacnunga (Old English medical compendium). Late 10th-early 11th century, Old English and Latin. View at http://www.bl.uk/manuscripts/Viewer.aspx?ref=harley_ms_585_f130r.
- Oxford, Bodleian MS Ashmole 1431: Pseudo-Apuleius Herbal. 11th century, Latin.
Other related manuscripts:
- London, BL Harley MS 6258 B: Old English Medical Miscellany, including Pseudo-Apuleius Platonicus; Herbarium; Medicina de quadrupedibus, with added medical recipes and remedies in Old English and Latin; Peri didaxeon. Late 11th century. View at http://www.bl.uk/manuscripts/FullDisplay.aspx?ref=Harley_MS_6258_b
[1] "Researchers from Nottingham Rediscover Anglo-Saxon AntiMicrobial," Society News, Society for General Microbiology, 31 Mar 2015, http://www.sgm.ac.uk/en/news/society-news.cfm.
[2] "Understanding Antimicrobial (Drug) Resistance," U.S. National Institutes of Health, 3 Apr 2012, http://www.niaid.nih.gov/topics/antimicrobialresistance/examples/mrsa/pages/default.aspx.
[3] M. L. Cameron, Anglo-Saxon Medicine (Cambridge: Cambridge University Press, 1993), 186.
[4] Thomas Oswald Cockayne, ed., Leechdoms, Wortcunning, and Starcraft of Early England, 3 vols. (London: Longman, 1864-66), II, 34.
[5] (trans. by Cockayne).
[6] Cameron, 119-20.
[7] Stephen Pollington, Leechcraft: Early English Charms, Plantlore and Healing (Hockwold, Norfolk: Anglo-Saxon Books: 2000).
[8] Carole Biggam offers an example of this difficulty by highlighting the term hæwenhnydele, which occurs eight different times in the OE corpus and is linked to the Latin plant name herba britannica. Scholars have been divided on how to interpret this term and exactly which plant it relates to. See "Hæwenhnydele: An Anglo-Saxon Medicinal Plant," Botanical Journal of Scotland 46.4 (1994).
[9] Barbara Brennessel, Michael D.C. Drout, and Robyn Gravel, "A Reassessment of the Efficacy of Anglo-Saxon Medicine," Anglo-Saxon England 34 (2005), 183-95.
[10] Ibid., 192.
[11] Linda E. Voigts, "Anglo-Saxon Plant Remedies and the Anglo-Saxons," Isis 70.2 (June 1979), 250-68. See especially pages 252-54. Anne Van Arsdall, Medieval Herbal Remedies: The Old English Herbarium and Anglo-Saxon Medicine (New York: Routledge, 2002), 35.
[12] Peter Dendle, "Lupines, Manganese, and Devil-Sickness: An Anglo-Saxon Medical Response to Epilepsy," Bulletin of the History of Medicine 75.1 (2001), 91-101. See especially page 91.
[13] Ibid., 100.
[14] Ibid., 97-98.
[15] Frances Watkins, Barbara Pendry, Olivia Corcoran, and Alberto Sanchez-Medina, "Anglo-Saxon Pharmacopoeia Revisited: A Potential Treasure in Drug Discovery," Drug Discovery Today 16:23/24 (December 2011), 1069-75.
[16] Ibid., 1071.
[17] Valerie Thomas, "Do Modern-Day Medical Herbalists Have Anything to Learn from Anglo-Saxon Medical Writings?," Journal of Herbal Medicine 1 (2011), 42-52.
[18] Marijane Osborn, "Anglo-Saxon Ethnobotany: Women's Reproductive Medicine in Leechbook III," Health and Healing from the Medieval Garden, ed. by Peter Dendle and Alain Touwaide (Woodbridge: Boydell, 2008), 145-61.
[19] Ibid., 150-51.
[20] Sarah Knapton, "Anglo-Saxon cow bile and garlic potion kills MRSA," The Telegraph, 30 Mar 2015, http://www.telegraph.co.uk/news/science/science-news/11504166/Anglo-Saxon-cow-bile-and-garlic-potion-kills-MRSA.html.
[21] [emphasis in the original] Kelly L. Bezio and Ashley Reed, "On the Limits of Disciplinarity: Literature, Medicine, Religion," Literature and Medicine 32.2 (Fall 2014), 240-48.
[6] Cameron, 119-20.
[7] Stephen Pollington, Leechcraft: Early English Charms, Plantlore and Healing (Hockwold, Norfolk: Anglo-Saxon Books: 2000).
[8] Carole Biggam offers an example of this difficulty by highlighting the term hæwenhnydele, which occurs eight different times in the OE corpus and is linked to the Latin plant name herba britannica. Scholars have been divided on how to interpret this term and exactly which plant it relates to. See "Hæwenhnydele: An Anglo-Saxon Medicinal Plant," Botanical Journal of Scotland 46.4 (1994).
[9] Barbara Brennessel, Michael D.C. Drout, and Robyn Gravel, "A Reassessment of the Efficacy of Anglo-Saxon Medicine," Anglo-Saxon England 34 (2005), 183-95.
[10] Ibid., 192.
[11] Linda E. Voigts, "Anglo-Saxon Plant Remedies and the Anglo-Saxons," Isis 70.2 (June 1979), 250-68. See especially pages 252-54. Anne Van Arsdall, Medieval Herbal Remedies: The Old English Herbarium and Anglo-Saxon Medicine (New York: Routledge, 2002), 35.
[12] Peter Dendle, "Lupines, Manganese, and Devil-Sickness: An Anglo-Saxon Medical Response to Epilepsy," Bulletin of the History of Medicine 75.1 (2001), 91-101. See especially page 91.
[13] Ibid., 100.
[14] Ibid., 97-98.
[15] Frances Watkins, Barbara Pendry, Olivia Corcoran, and Alberto Sanchez-Medina, "Anglo-Saxon Pharmacopoeia Revisited: A Potential Treasure in Drug Discovery," Drug Discovery Today 16:23/24 (December 2011), 1069-75.
[16] Ibid., 1071.
[17] Valerie Thomas, "Do Modern-Day Medical Herbalists Have Anything to Learn from Anglo-Saxon Medical Writings?," Journal of Herbal Medicine 1 (2011), 42-52.
[18] Marijane Osborn, "Anglo-Saxon Ethnobotany: Women's Reproductive Medicine in Leechbook III," Health and Healing from the Medieval Garden, ed. by Peter Dendle and Alain Touwaide (Woodbridge: Boydell, 2008), 145-61.
[19] Ibid., 150-51.
[20] Sarah Knapton, "Anglo-Saxon cow bile and garlic potion kills MRSA," The Telegraph, 30 Mar 2015, http://www.telegraph.co.uk/news/science/science-news/11504166/Anglo-Saxon-cow-bile-and-garlic-potion-kills-MRSA.html.
[21] [emphasis in the original] Kelly L. Bezio and Ashley Reed, "On the Limits of Disciplinarity: Literature, Medicine, Religion," Literature and Medicine 32.2 (Fall 2014), 240-48.